
[ad_1]
In a latest research printed within the journal PNAS, a bunch of researchers developed an intranasal measles-mumps-SARS-CoV-2 spike (S) protein (MMS) vaccine that gives broad, sturdy safety in opposition to main Extreme Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) variants, leveraging the confirmed security of the measles-mumps-rubella (MMR) vaccine platform.
 Research: A next-generation intranasal trivalent MMS vaccine induces sturdy and broad safety in opposition to SARS-CoV-2 variants of concern. Picture Credit score: TopMicrobialStock / Shutterstock
Research: A next-generation intranasal trivalent MMS vaccine induces sturdy and broad safety in opposition to SARS-CoV-2 variants of concern. Picture Credit score: TopMicrobialStock / Shutterstock
Background
The coronavirus illness 2019 (COVID-19) pandemic, triggered by SARS-CoV-2, has led to over 6.96 million deaths and greater than 771 million infections globally as of October 2023. Though a number of vaccines utilizing the prefusion spike (S) protein as an immunogen have been developed, they’ve limitations like lowered effectiveness in opposition to evolving SARS-CoV-2 variants, short-lived safety, and lack of mucosal immunity. The emergence of varied variants, particularly the Omicron with quite a few mutations, poses challenges to present vaccines’ effectiveness. Given this, there’s a urgent want for more practical vaccines. Given the persistent emergence of SARS-CoV-2 variants and the constraints of present vaccines, additional analysis is required for next-generation intranasal vaccines that present broader mucosal immunity and are adaptable to evolving strains.
Concerning the research
The analysis delved into the excellent evaluation and improvement of modified measles and mumps viruses (recombinant Measles Virus (rMeV), recombinant Mumps Virus (rMuV-JL1), and rMuV-JL2) that specific the SARS-CoV-2 six prolines (preS-6P) proteins. Procedures for progress curves, virus preparation, purification, and varied assays have been applied. These assays embody Measles Virus (MeV), Mumps Virus (MuV), and SARS-CoV-2 plaque assessments, ribonucleic acid (RNA) extraction, Reverse Transcription Polymerase Chain Response (RT-PCR), and Western blotting, amongst others. The Ohio State College’s Institutional Laboratory Animal Care and Use Committee authorised the animal research, referencing protocol numbers 2009A1060-R3 and 2020A00000053. Animal testing concerned immunizing and difficult IFNAR1−/− mice and golden Syrian hamsters.
Additional steps within the research detailed protein purification, T cell assays, circulation cytometry, and Enzyme-Linked Immunosorbent Assay (ELISA) assessments to detect particular SARS-CoV-2 Immunoglobulin G (IgG) and Immunoglobulin A (IgA) antibodies. Additionally they explored SARS-CoV-2’s neutralizing skill, pseudotype neutralization, and the willpower of SARS-CoV-2 focus in animal tissues. Histological examinations have been carried out, and all outcomes underwent statistical evaluation.
Research outcomes
Researchers not too long ago discovered that the preS stabilized with preS-6P induced a better neutralizing antibody response than one other variant. The preS-6P gene of the SARS-CoV-2 Delta variant was then built-in into a special genome. This altered pressure differed in progress and mobile results however maintained robust protein expression, much like the Delta variant. A gene from the SARS-CoV-2 Omicron BA.1 was additionally built-in right into a separate vaccine genome with comparable observations.
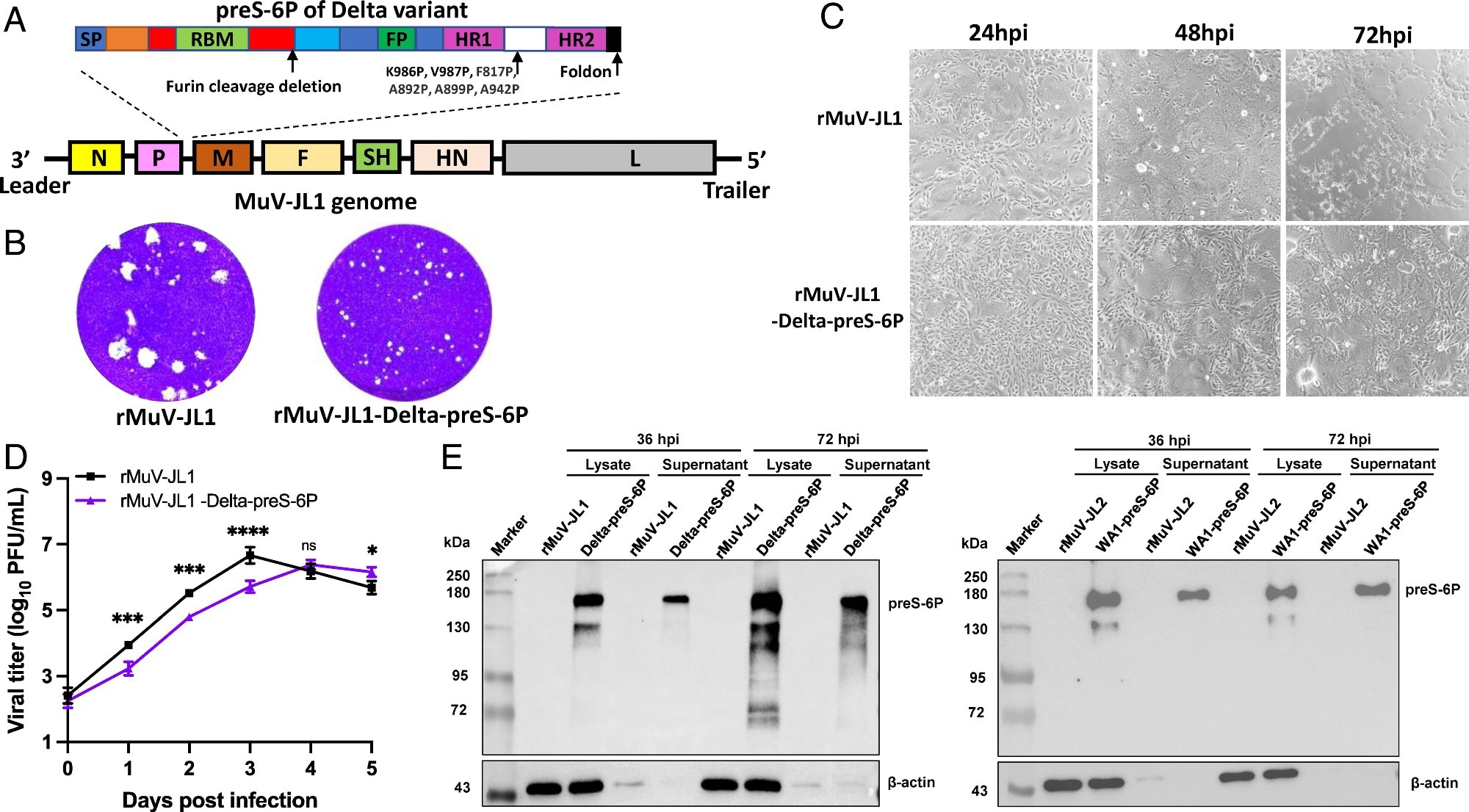 Restoration and characterization of rMuV-JL1-Delta-preS-6P expressing the six proline-stabilized prefusion spike of SARS-CoV-2 Delta variant. (A) Technique for insertion of preS-6P of the Delta variant into the P and M gene junction within the MuV-JL1 genome. (B) The plaque morphology of rMuV-JL1 and rMuV-JL1-Delta-preS-6P in Vero CCL81 cells at day 5. (C) rMuV-JL1-Delta-preS-6P displays delayed syncytia formation in Vero CCL81 cells (MOI of 0.1). (D) Replication kinetics of recombinant viruses in Vero CCL81 cells at an MOI of 0.1. (E) Expression of preS-6P in rMuV-JL1-Delta-preS-6P (Left) or rMuV-JL2-WA1-preS-6P (Proper)-infected Vero CCL81 cells. An MOI of 0.1 was used for an infection, and 10 μL of cell lysate (from whole 200 μL) and 10 μL (from whole 1 mL) of supernatant have been used for Western blot.
Restoration and characterization of rMuV-JL1-Delta-preS-6P expressing the six proline-stabilized prefusion spike of SARS-CoV-2 Delta variant. (A) Technique for insertion of preS-6P of the Delta variant into the P and M gene junction within the MuV-JL1 genome. (B) The plaque morphology of rMuV-JL1 and rMuV-JL1-Delta-preS-6P in Vero CCL81 cells at day 5. (C) rMuV-JL1-Delta-preS-6P displays delayed syncytia formation in Vero CCL81 cells (MOI of 0.1). (D) Replication kinetics of recombinant viruses in Vero CCL81 cells at an MOI of 0.1. (E) Expression of preS-6P in rMuV-JL1-Delta-preS-6P (Left) or rMuV-JL2-WA1-preS-6P (Proper)-infected Vero CCL81 cells. An MOI of 0.1 was used for an infection, and 10 μL of cell lysate (from whole 200 μL) and 10 μL (from whole 1 mL) of supernatant have been used for Western blot.
A trivalent vaccine was developed and examined in opposition to a single-strain vaccine in mice from these modified viruses. The trivalent vaccine led to a broader immune response, producing neutralizing antibodies in opposition to a number of SARS-CoV-2 variants. Each vaccines maintained antibody responses for 4 months and stimulated tissue-resident reminiscence T cell responses within the lungs, crucial for SARS-CoV-2 protection. Nevertheless, the trivalent model confirmed a extra complete protecting capability.
Seven weeks post-immunization, T-cell responses have been analyzed within the mice’s splenocytes. The trivalent vaccine activated T-helper 1 (Th1) cells greater than its monovalent counterpart and notably stimulated extra Interleukin-4 (IL-4)-producing T helper cells. Each vaccines incited important numbers of T helper cells producing IL-21 and IL-17. Nonetheless, the trivalent model demonstrated a superior systemic T-cell immune response.
In experiments utilizing Golden Syrian Hamsters, the trivalent vaccine exhibited broader neutralizing exercise in opposition to varied SARS-CoV-2 variants. In distinction, the monovalent vaccine was extra particular to the Omicron BA.1 variant. When uncovered to SARS-CoV-2, the trivalent vaccine provided enhanced safety, particularly in opposition to the WA1 and Delta strains.
Moreover, intranasal administration of the trivalent vaccine in separate assessments supplied full SARS-CoV-2 safety and triggered a stronger serum IgG antibody response in comparison with subcutaneous administration. Intranasal supply additionally led to a potent mucosal IgA antibody response, not seen within the subcutaneous group. This means that the supply methodology can considerably impression immune responses, with intranasal immunization probably providing superior safety in opposition to respiratory viruses like SARS-CoV-2.
Conclusions
To summarize, researchers developed an intranasal trivalent MMS vaccine that may fight measles, mumps, and varied SARS-CoV-2 variants. The vaccine was noticed to supply robust systemic and lung-specific immune responses, providing safety in opposition to a number of SARS-CoV-2 strains, together with the Delta and Omicron BA.1 variants. This trivalent vaccine is a modified model of the MMR vaccine and showcases broad neutralizing capabilities in opposition to a number of virus strains, in distinction to monovalent vaccines, that are restricted of their protecting scope. Intranasal administration of the MMS vaccine induces robust immune responses each systemically and within the mucosal areas, probably providing superior safety in opposition to SARS-CoV-2 variants. Importantly, the vaccine’s design permits for straightforward modifications to handle newly rising variants. In essence, this next-generation COVID-19 vaccine candidate demonstrates broad and sturdy safety, highlighting its potential as a big software in opposition to SARS-CoV-2 variants.
[ad_2]